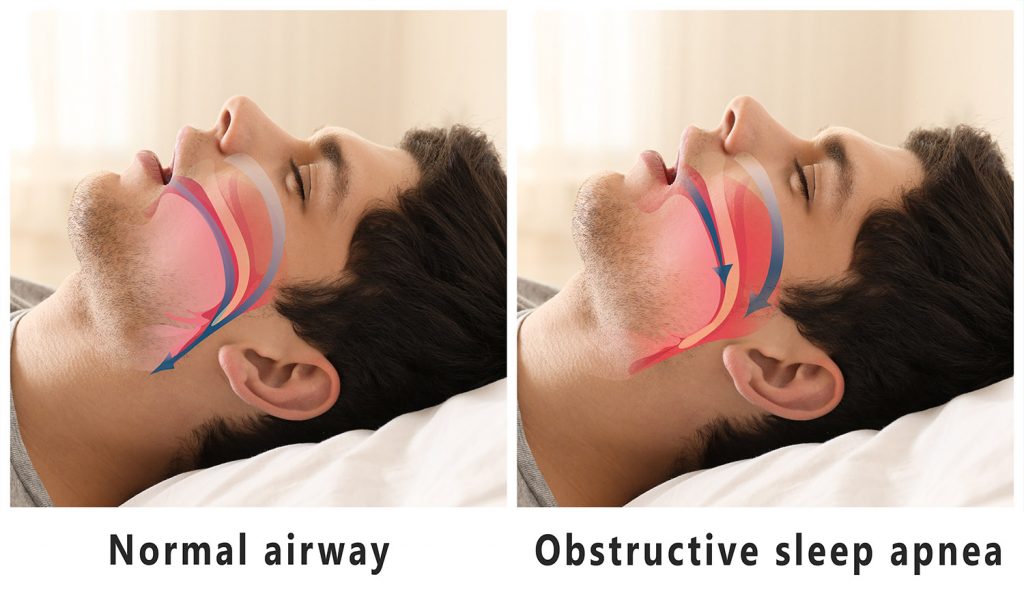
Sleep Disordered Breathing (SDB) describes a group of disorders that are related to breathing abnormalities during sleep. SDB includes several disorders related to a compromised airway including:
• Snoring
• Upper Airway Resistance Syndrome (UARS)
• Obstructive Sleep Apnea (OSA)
To many, snoring is natural, and although it can be annoying to some, they don’t seek medical attention to treat it. Snoring could eventually lead to SDB, which can then lead to OSA.
Snoring is the most common symptom of SDB. The International Classification of Sleep Disorders Diagnostic and Coding Manual defines snoring as, “a respiratory sound generated in the upper airway during sleep that typically occurs during inspiration but may also occur in expiration, without episodes of apnea or hypoventilation.” Although snoring is characterized by periods of no breathing or periods of oxygen decrease, it can lead to SDB. Snoring can be treated with an oral device and eventually eliminated. Having the oral device as a part of treatment reduces the risk of someone’s snoring developing into more sever SDB.
UARS is often confused with OSA, but there are distinctive differences. With UARS, there is no decrease in oxygen concentration and no apneic events occur. People find them to be very similar because during UARS, there is enough resistance of airflow that it causes a person to be awakened from their sleep because of short episodes that trigger movement. These episodes are referred to as respiratory effort-related arousals (RERAs). Many people don’t notice the amount of times they are actually being interrupted during their sleep, which can cause them to feel exhausted during the day.
OSA, also known as Obstructive Sleep Apnea-Hyponea Syndrome (OSAHS), is very similar to UARS. During both, airway obstruction leads to the person to experience the episodes that trigger movement and cause the person to be awaken from the normal sleep pattern. But with OSA, partial (hypopnea) or complete (apnea) cessation of airflow occurs. There are so many people who suffer from OSA, but aren’t diagnosed properly. A proper diagnosis is critical because if untreated, it could lead to an increased risk of high blood pressure, heart disease, diabetes, and stroke.